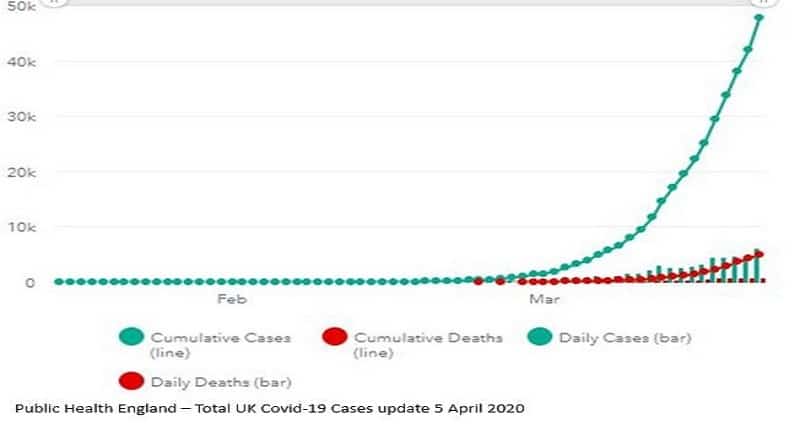
The Board of Deputies of British Jews is liaising with six of the largest denominational burial boards and the Orthodox burial boards in Manchester to collate an indicator of deaths where COVID-19 was a factor. Its latest report (3 April) said there had been 85 Jewish funerals carried out where the deceased contracted Covid-19. The Department of Health figures from 5 April indicated the total number of UK death from coronavirus was 4,934.
Professor David Katz, executive chairman of the Jewish Medical Association, offers a view:
Are Jews over-represented amongst those who have died from SARS-Cov-2 infection in the UK? If so, why?
Arguments are that:
- in the initial phase of the UK pandemic there were many Jews who died – vastly in excess of roughly 0.5%, which is the accepted percentage of Jews in the country
- there were well publicised large social and religious gatherings in the UK Jewish community, up to and including the first 3.5 weeks of March, some coinciding with the festival of Purim; and many synagogues, study centres and other Jewish activities continued as always, particularly but not exclusively in strictly observant areas, which promoted the spread of the virus
- the suggestion has been made that in fact the strictly orthodox do not care and obstinately refused to adapt their lifestyles because of lack of respect for secular authority
- this view links in to similar over-representation, and event reports, about the strictly observant Jewish sector in Israel, and in the USA – particularly in New York, which has a very high Jewish population
- the large family size in the strictly observant Jewish sector can amplify the virus spread internally amongst the community, and as a result externally into wider society
- the Jewish community as a whole, like many other faith communities – has an emphasis on community activity, whether religious or cultural celebrations, social action, or communal prayer; this is intergenerational – thus over 70s regular mix with young children as opposed to isolated or lonely pensioners, who may not mingle with youth during a normal week
- some specific Jewish practices – mikva (ritual bathing), social gatherings for Milah (traditional neonatal male circumcision), practices around handling of the body after death, shiva (bereavement practices) – are likely to be associated with infection risk, either for the individual or for the group
However, there are arguments against:
- the initial epicentre of the UK pandemic was in London, and it is in London that the majority of Jews are based, so one might expect them to be affected more than others during this initial period
- as a demographic the Jewish community is older than the rest of the UK population so there will inevitably be more of them in an at risk group
- at one point Jewish deaths were 6% of the total UK – today they are 2.3% of the total – now the total number of deaths is far higher than it was, so the denominator matters significantly
- the comparison has been made for the Jewish community – it has not been made with other minority faith and ethnic communities – Cypriot, Hindu, Irish Catholic, Muslim, Sikh
- there are religious gatherings and communal activities continuing in other faith communities, which may yet lead to higher death rates – but thus far this has not been described in the UK, so one would have to postulate a specific Jewish effect?
- there is always the question of Jewish definition – who is counted in this data?
- are there any differences in the Jewish versus other “cases” and how are Jews represented in screening? All such analysis is hampered by lack of adequate information about the baseline – at present testing is only being done nationally in hospitals. Without far more testing there is no satisfactory indication of prevalence of infection (“cases”?) in either the wider or the Jewish population; or about the real prevalence of symptoms amongst those infected. Modelling may be outstanding and has guided the current management and restrictions but applying it to societal subgroups may not be staightforward
- there has been self-scrutiny of Jewish practices, and new limitations introduced have confronted with the need for self–isolation, use of protective clothing, etc – but these have been formulated as preventive measures rather than as a response to known episodes of infection
- there are parts of the strict orthodox community where access to conventional and social media is limited and thus may not be aware of current news
- there are Jewish practices – again found in the strictly orthodox mainly but not exclusively – which are regarded as expendable / obsolete / even primitive, and therefore one has to distinguish between saying they should be abandoned forthwith because of such prejudice, rather than because they spread disease